Abstract
Older patients are at increased risk for complications and death following allogeneic hematopoietic cell transplantation (allo-HCT). Traditional transplant-specific prognostic indices such as hematopoietic cell transplant comorbidity index (HCT-CI) may not capture all underlying geriatric vulnerabilities, and in-depth evaluation by a geriatrician prior to transplant may not always be available. We hypothesize that routine pre-transplant assessments by interdisciplinary clinical providers including advanced practice providers, nursing staff, physical therapists, occupational therapists, and dietitians, as well as common laboratory tests, may uncover additional geriatric deficits.
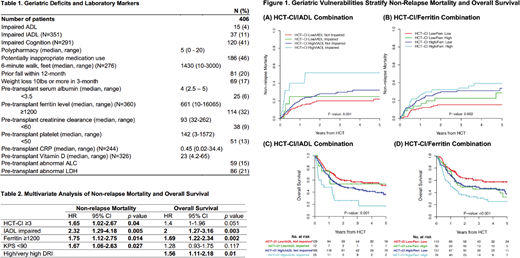
Using an institutional database and the electronic medical records of 406 adults age 60 years and older (range 60-78.7) who underwent first allo-HCT for hematological malignancies from 2010 to 2016, we examined the prevalence and the prognostic impact of pre-transplant geriatric deficits identified by interdisciplinary clinical providers including geriatric domains of functional activity, cognition, medication, nutrition, and mobility (Table 1), and by routine laboratory tests. With a median follow-up of 39 months for survivors, the 3-year probability of overall survival (OS) and progression-free survival was 47% (95% CI 42-53) and 40% (95% CI 35-45), respectively. The 2-year cumulative incidence of non-relapse mortality (NRM) was 26% (95% CI 22-29). Among pre-transplant geriatric and laboratory variables, we found that impairment in instrumental activities of daily living (IADL) and pre-transplant ferritin level ≥1200 was independently associated with increased NRM and inferior OS. In the multivariate analysis, HCT-CI ≥3, IADL impairment, ferritin level ≥1200, and Karnofsky Performance Scale (KPS) <90 are predictive of NRM (Table 2). Similarly, IADL impairment, ferritin level ≥1200, and high/very high modified disease risk index predict OS (Table 2).
Most importantly, the combination of either IADL impairment or ferritin ≥1200 with HCT-CI further stratifies NRM and OS into distinct risk categories, including a group of highly vulnerable, high risk patients with high HCT-CI (≥3) plus IADL impairment and/or ferritin level ≥1200 (Figure 1). Detailed examination of non-relapse death among all vulnerable patients (≥2 risk factors) reveals a higher proportion of death from organ toxicities than patients with zero or 1 risk factor. Our findings establish a rapid and simple assessment tool to risk stratify older patients prior to allo-HCT. While requiring validation, the geriatric vulnerability index can be easily completed and integrated into outpatient clinics and the electronic medical record. It may also provide an entry point for prospective, interventional trials aimed at reducing non-relapse mortality and toxicities, and at improving survival and quality of life of older allo-HCT patients.
Perales:Takeda: Other: Personal fees; Merck: Other: Personal fees; Incyte: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees and Clinical trial support; Abbvie: Other: Personal fees; Novartis: Other: Personal fees. Sauter:Juno Therapeutics: Consultancy, Research Funding; Sanofi-Genzyme: Consultancy, Research Funding; Spectrum Pharmaceuticals: Consultancy; Novartis: Consultancy; Precision Biosciences: Consultancy; Kite: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal